Did you know that April is Autism Awareness Month? As research and awareness grows around the neurodiversity paradigm, links between eating disorders and neurodivergent individuals and subsequent approaches to treatment are also evolving. Currently, most research is focused on the links between autism and two types of eating disorders; anorexia nervosa and ARFID. Research shows that approximately 37% of individuals with anorexia nervosa are autistic. ADHD, another neurodevelopmental phenomenon, has also been correlated with bingeing and purging eating disorder subtypes such as bulimia nervosa, as well as binge eating disorder.
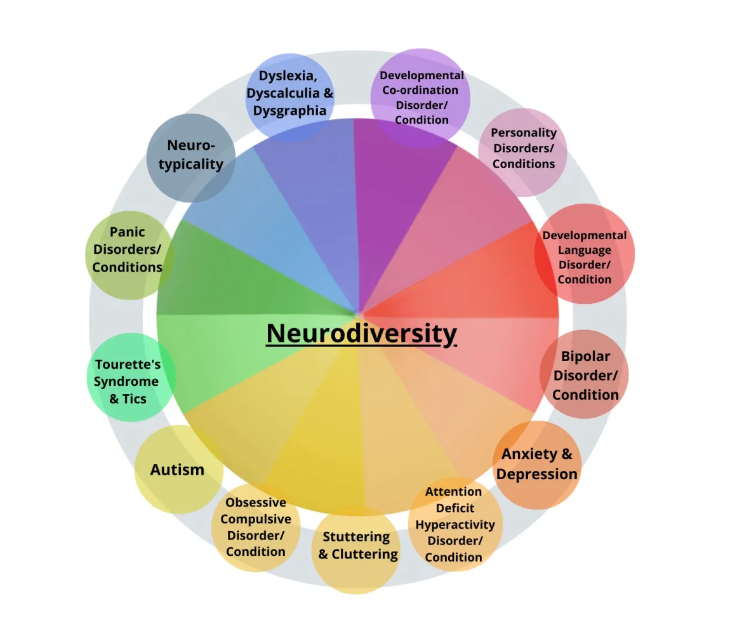
Remember, Autism is just one neurotype or neurodevelopmental phenomenon! Image source: https://stimpunks.org/glossary/neurodiversity/