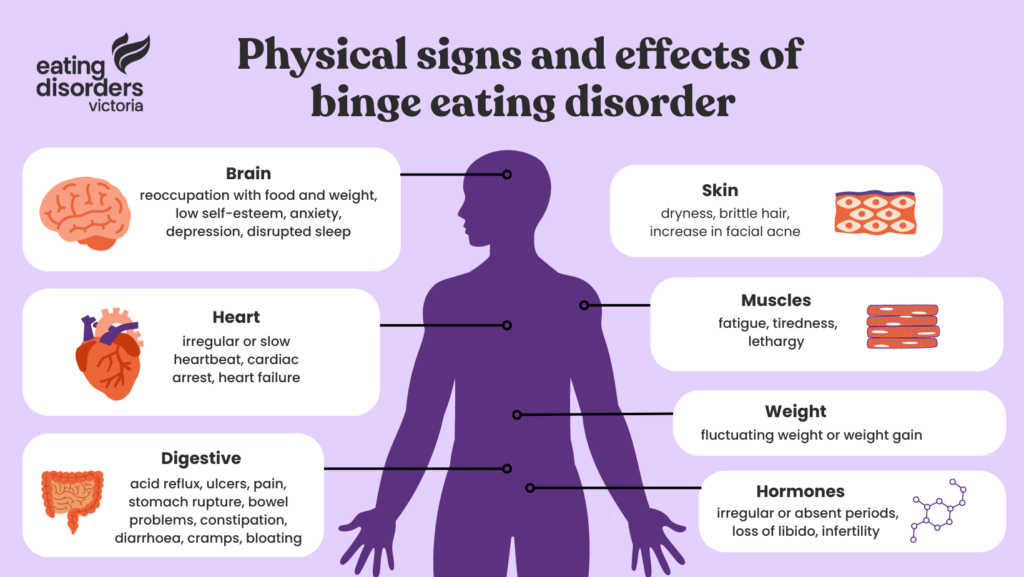
Binge eating disorder (BED) is a mental illness characterised by regular episodes of binge eating. Binge eating involves eating an excessive amount of food, which may take place in a rapid space of time or may be more of an extended grazing. These episodes can feel chaotic, uncontrollable and highly distressing.
During a binge eating episode, a person may not be hungry, but may continue to eat past the point of feeling comfortably full. It is common for people to binge eat alone or in secret, and experience intense feelings of guilt, shame, disgust and low mood after a binge. When identifying binge eating disorder, it’s important to remember that:
- BED is a serious mental illness which affects more people than any other eating disorder
- BED affects men and women roughly equally
- BED can present differently for different people and impacts people in all body shapes and sizes
- BED can often be downplayed as ‘emotional eating’, which can prevent people from seeking help
- BED is serious and requires professional support
How is a binge different to overeating?
Overeating is part of being human – we can overeat naturally in social settings (e.g., Christmas lunch) or alone (e.g., a night in with Netflix and takeaway). By choice or accident, overeating is when someone eats past the point of comfortably full. We may overeat because food is present, because the food we are eating is pleasurable, we are bored or distracted, or because it soothes or comforts us (e.g., when feeling sad, overwhelmed or after a tough day).
A binge is different from overeating and is far more pervasive. It is the intense drive to overeat which is experienced again and again over time, accompanied by feelings of shame, guilt and feeling out of control. Binge eating is highly distressing and can affect a person’s ability to engage fully in aspects of life (e.g., work or school, recreational activities, socialising and relationships).
Similarities with bulimia nervosa
Binge eating disorder is similar to — but not the same — as bulimia nervosa. Where people experiencing bulimia nervosa will engage in compensatory activities after a binge eating episode (such as self-induced vomiting, fasting, over-exercising and/or the misuse of laxatives, enemas or diuretics), Binge eating disorder is characterised by an absence of compensatory activities, despite experiencing similar feelings of intense guilt, shame and self-hatred after a binge episode.
Like people with bulimia nervosa, there may be a strong desire to “make up” for the binge by being “good”, “healthy” or punishing oneself. This can lead to restrictive eating by engaging in long term dieting and sporadic fasts after a binge.