Avoidant/restrictive food intake disorder (ARFID) is the sensory based avoidance, fear or restriction of certain foods, due to sensitivities to texture, smell, temperature, or appearance of the food.
A person may restrict the amount or type of a particular food or avoid a particular food based on factors such as the appearance of the food (e.g., colour, size, shape), texture, smell, temperature, or food group (e.g., all vegetables after a bad experience choking on a vegetable). They may also restrict food intake due to early satiety (i.e., prematurely feels full) or due to past experiences, such as trauma associated with a food experience (e.g., choking).
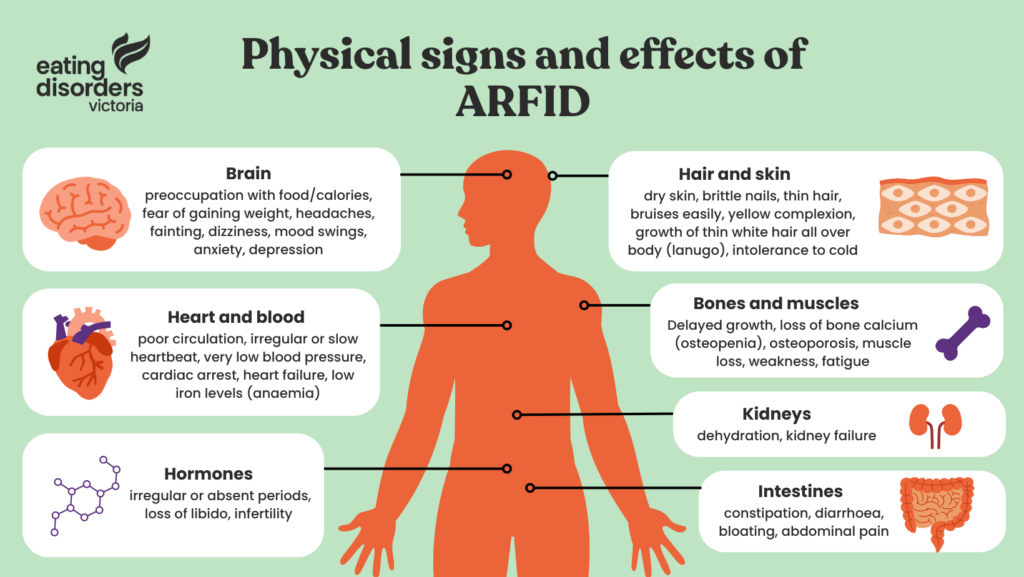
Defined by a pattern of eating that is limited in variety (e.g., avoidance of specific foods) and/or volume (e.g., restriction of amount), ARFID can cause a person to become seriously ill because their bodies aren’t getting all the nutrients they need. For example, individuals may experience medical or mental health consequences such as poor growth, diabetes, cardiovascular disease, fatigue, poor self-esteem, family mealtime conflict, peer social isolation, and difficulties with school, relationships and work.
While ARFID is similar to anorexia nervosa in that a person restricts their food intake, the intent or reason for restricting food intake differs between the two eating disorders. People with ARFID do not restrict food to avoid weight gain/control weight or to change their body size/shape. ARFID is not associated with weight or shape concerns – weight loss or change in shape may occur as a result of poor nutritional intake, not because a person is intentionally engaging in weight control behaviours.
How does ARFID present?
Individuals of all ages and genders can have clinically significant avoidant/restrictive eating that does not always begin in early childhood. Importantly, food avoidance/restriction does not always or only lead to weight loss. Depending on food intake (type and amount) and reliance on tube feeding/oral supplements, ARFID is experienced by individuals across the weight spectrum.
How is ARFID diagnosed?
Diagnosis is associated with at least one of the following:
(1) Significant weight loss (or failure to achieve weight gain/physical growth in children);
(2) Significant nutritional deficiency;
(3) Dependence on tube feeding (supplying nutrients directly to the gastrointestinal tract) or oral nutritional supplements;
(4) Marked interference on an individual’s psychosocial functioning (e.g., impacts on daily activities).
Diagnosis is made if symptoms are not better explained by a concurrent medical condition (e.g., allergies, intolerances, other medical conditions), other mental illness (including other eating disorders, such as Anorexia Nervosa), a lack of available food or a cultural practice (e.g., Ramadan). ARFID differs from picky or fussy eating, which is common in childhood and generally resolves over time (e.g., food neophobia).
The food avoidance and restriction that define ARFID can lead to medical or mental health consequences that further exacerbate food avoidance and restriction and serve to maintain the illness. ARFID is persistent, more severe, can involve the restriction of both familiar and new foods, and has significant physical and mental health consequences.